The “Texas Breather”: TTUHSC El Paso and UTEP Develop a Low-Cost, 3D-Printed Ventilator for Hospitals
Last Updated on June 25, 2020 at 12:00 AM
Originally published June 25, 2020
By UC Staff
UTEP Communications
EL PASO, Texas – Nationwide, hospitals are concerned about a possible shortage of ventilators as more Americans require treatment for COVID-19, the novel coronavirus disease that can cause life-threatening respiratory problems such as pneumonia.
A collaboration between Texas Tech University Health Sciences Center El Paso and The University of Texas at El Paso could help solve the problem. Using 3D printing, the team of physicians and engineers have developed an innovative, low-cost ventilator for the health care sector.
Scott Crawford, M.D., associate professor and director of TTUHSC El Paso’s Training and Educational Center for Healthcare Simulation (TECHS), is helping lead the initiative to manufacture the shoebox-sized devices, dubbed the Texas Power Bag Breather, or Texas Breather.
“This low-cost ventilator would be used if existing mechanical ventilators were not available in any setting requiring assisted breathing,” Dr. Crawford said. “While there’s a particular need in third-world and developing nations, if an industrialized nation became overwhelmed, it could help in those regions as well.”
The Texas Breather design was developed by Dr. Crawford; retired TTUHSC El Paso faculty member Robert Stump, M.D., Ph.D.; and Luis Ochoa, a manager at the W.M. Keck Center for 3D Innovation in UTEP’s College of Engineering. After two weeks of prototyping six iterations of the device, Ochoa requested support from UTEP Keck Center Director Ryan Wicker, Ph.D., to put the full resources of the center behind the project.
“Dr. Crawford, Dr. Stump and Luis converged on a simple, yet elegant and innovative concept that capitalized on the strengths of additive manufacturing,” Wicker said. “Recognizing the need and the potential clinical advantages of the design, this was a perfect application of the Keck Center’s rapid-response engineering capabilities. More than a dozen individuals, including faculty, staff and students, immediately focused 100% effort on getting the design finalized for reliability testing. We combined simulation, design interaction, and rapid prototyping and testing to respond in a pandemic timescale. I am very proud of Luis and the entire Keck team for how quickly we came together to try and make a difference during this pandemic.”
The team has requested an emergency use authorization (EUA) from the U.S. Food and Drug Administration to allow health care workers to use the Texas Breather during the COVID-19 pandemic.
Hospital ventilators can cost tens of thousands of dollars, but Dr. Crawford believes the Texas Breather can be made using currently available 3D technology for less than $1,000 per unit, thanks to the design’s simplicity. He said each device would take about eight hours to produce.
The main cost-and-time saving innovation of the Texas Breather involves the incorporation of relatively inexpensive bag-valve mask devices that are available in large quantities at hospitals. First responders and emergency health care teams use bag-valve masks to manually provide ventilation to patients who are not breathing or are having trouble breathing.
Close collaboration between the TTUHSC El Paso board-certified emergency physicians and their teams, and the faculty, engineers and students in the Keck Center at UTEP was key to rapidly refining the design of the Texas Breather. The device mounts to an IV pole at the patient’s bedside and provides an adjustable airflow volume and respiratory rate. All mechanical components are fabricated with production-grade material and have successfully passed simulated-use and worst-case scenario testing.
The team used advanced respiratory simulation tools in the TECHS center to test and calibrate the device. These tools, used by TTUHSC El Paso students to study respiratory physiology, played an important part in validating the safety and functionality of the Texas Breather.
“Being able to accurately record the pressure, volume and airflow of the Texas Breather was a key element for pursuing emergency use authorization from the FDA. We’re fortunate to have access to these specialty simulation tools at TECHS,” Dr. Crawford said.
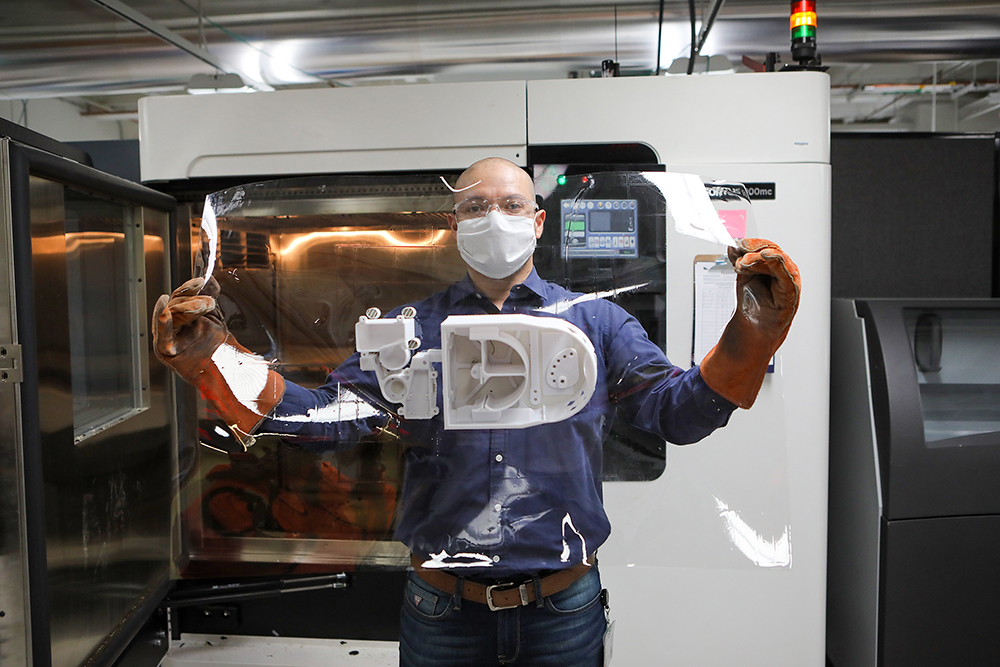
UTEP used a Stratasys 3D printer to produce parts to assemble the Texas Breather devices. Dr. Crawford said the team has produced working prototypes, and with additional funding, large-scale production using 3D printing could produce hundreds per week.
Ochoa, who has been working with Stratasys equipment for nearly two decades, translated the doctors’ design concepts into reality. The team used computer simulation to refine the design, which reduced the number of design-build-test cycles and shortened the development process by weeks. This expertise in UTEP’s Keck Center in close collaboration with the TTUHSC El Paso doctors was the key to success.
Key industry partners of the Keck Center also contributed to the development of the Texas Breather. Medical device professionals from Bessel LLC helped prepare for FDA submission, simulation software maker Ansys Inc. assisted UTEP engineers with extensive simulations, and Stratasys Inc. donated prototypes and materials for fabrication.
Stormy Monks, Ph.D., assistant professor in the Foster School of Medicine’s Department of Emergency Medicine at TTUHSC El Paso, and Jesica Urbina, Ph.D., TECHS senior research associate, are working to secure grants to support production of the Texas Breather. Victor Torres, TECHS innovation engineer, and Joel Libove, Ph.D., are assisting in the final design of electrical controls for the ventilator.
“We have the goal of sharing our invention for general use but are pursuing grant funding for manufacturing on a large scale,” Dr. Crawford said. “We would like to produce 1,000 to 2,000 units to assist with the projected deficit of ventilators in American hospitals.”
